Emerging Strategies in the Management of Heart Failure with Preserved Ejection Fraction: Integrating SGLT2 Inhibitors, Lifestyle Interventions, and Multidisciplinary Care
DOI:
https://doi.org/10.56532/mjsat.v5i4.587Keywords:
HFpEF, Lifestyle interventions, Multidisciplinary care, SGLT2 inhibitors, Symptom managementAbstract
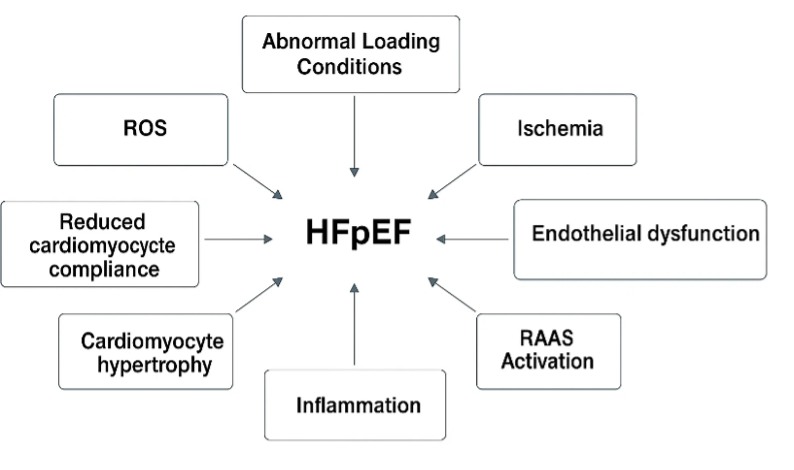
Heart failure with preserved ejection fraction (HFpEF) is a complex clinical syndrome characterized by heart failure symptoms despite a left ventricular ejection fraction ≥50%, representing about 50% of all heart failure cases. Its increasing prevalence, driven by an aging population and comorbidities like hypertension, diabetes, and obesity, poses significant challenges due to frequent hospitalizations, impaired quality of life, and high mortality rates. The pathophysiology of HFpEF is multifactorial, involving systemic inflammation, endothelial dysfunction, myocardial fibrosis, and increased ventricular stiffness, indicating a systemic syndrome requiring a multidisciplinary treatment approach. While current guidelines emphasize symptom relief, comorbidity management, and lifestyle changes, the emergence of sodium-glucose cotransporter 2 (SGLT2) inhibitors has revolutionized HFpEF management. Large randomized controlled trials like EMPEROR-Preserved and DELIVER have demonstrated their ability to significantly reduce heart failure hospitalizations and improve quality of life. Additionally, structured exercise training, dietary modifications, and behavioral support have shown benefits in enhancing functional capacity and overall well-being. Multidisciplinary care models involving collaboration among various healthcare professionals have the potential to optimize patient-centered care and improve outcomes. However, challenges persist, including the heterogeneity of HFpEF phenotypes, underrepresentation of high-risk populations in trials, and inconsistent implementation of lifestyle and multidisciplinary interventions. Future directions should focus on personalized treatment strategies guided by deep phenotyping and biomarkers, equitable access to care, and the integration of pharmacological therapies with scalable lifestyle interventions and technology-enabled monitoring systems. Addressing these issues will be crucial in alleviating the global burden of HFpEF and improving patient outcomes.
References
B. Bozkurt, A. Coats, H. Tsutsui, et al., “Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure,” Journal of Cardiac Failure, 2021. https://doi.org/10.1016/j.cardfail.2021.01.022
P. Campbell, F. H. Rutten, M. M. Lee, N. M. Hawkins, and M. C. Petrie, “Heart failure with preserved ejection fraction: everything the clinician needs to know,” The Lancet, vol. 403, no. 10431, pp. 1083-1092, 2024.
A. Jasinska-Piadlo and P. Campbell, “Management of patients with heart failure and preserved ejection fraction,” Heart, vol. 109, no. 11, pp. 874-883, 2023. https://doi.org/10.1136/heartjnl-2022-321097
A. B. Gevaert, R. Kataria, F. Zannad, et al., “Heart failure with preserved ejection fraction: recent concepts in diagnosis, mechanisms and management,” Heart, vol. 108, no. 17, pp. 1342-1350, 2022. https://doi.org/10.1136/heartjnl-2021-319605
A. Mahmood, E. Dhall, C. P. Primus, et al., “Heart failure with preserved ejection fraction management: a systematic review of clinical practice guidelines and recommendations,” European Heart Journal – Quality of Care and Clinical Outcomes, vol. 10, no. 7, pp. 571-589, 2024. https://doi.org/10.1093/ehjqcco/qcae053
P. Mołek-Dziadosz and J. Nessler, “Heart failure with preserved ejection fraction as an interdisciplinary problem,” Journal of Medical Research, vol. 77, no. 1, p. 17944, 2025. https://doi.org/10.20452/jmr.2025.17944
P. P. Toth and D. Gauthier, “Heart failure with preserved ejection fraction: strategies for disease management and emerging therapeutic approaches,” Postgraduate Medicine, vol. 133, no. 2, pp. 125-139, 2021. https://doi.org/10.1080/00325481.2020.1842620
M. Agarwal and S. N. Pakhare, “Emerging therapeutic strategies in heart failure management: a narrative review of current evidence and future directions,” International Journal of Cardiovascular Sciences, vol. 6, no. 1, pp. 32-38, 2024. https://doi.org/10.33545/26649020.2024.v6.i1a.47
FNU Sapna, FNU Raveena, M. Chandio, et al., “Advancements in heart failure management: a comprehensive narrative review of emerging therapies,” Cureus, vol. 15, no. 10, e46486, 2023. https://doi.org/10.7759/cureus.46486
M. M. Hammond, I. K. Everitt, and S. S. Khan, “New strategies and therapies for the prevention of heart failure in high‐risk patients,” Clinical Cardiology, vol. 45, suppl. 13, pp. S13-S25, 2022. https://doi.org/10.1002/clc.23839
M. Sweeney, B. Corden, and S. Cook, “Targeting cardiac fibrosis in heart failure with preserved ejection fraction: mirage or miracle?” EMBO Molecular Medicine, vol. 12, no. 12, e10865, 2020. https://doi.org/10.15252/emmm.201910865
S. Zhazykbayeva, S. Pabel, A. Mugge, et al., “The molecular mechanisms associated with the physiological responses to inflammation and oxidative stress in cardiovascular diseases,” Biophysical Reviews, vol. 12, pp. 947-968, 2020. https://doi.org/10.1007/s12551-020-00742-0
J. B. Echouffo-Tcheugui, S. Lewsey, and R. Weiss, “SGLT2 inhibitors: further evidence for heart failure with preserved ejection fraction as a metabolic disease?” Journal of Clinical Investigation, vol. 131, no. 23, e156309, 2021. https://doi.org/10.1172/JCI156309
A. B. De Lorenzi, E. Kaplinsky, M. R. Zambrano, L. T. Chaume, and J. M. Rosas, “Emerging concepts in heart failure management and treatment: focus on SGLT2 inhibitors in heart failure with preserved ejection fraction,” Drugs in Context, vol. 12, 2022-7-1, 2023. https://doi.org/10.7573/dic.2022-7-1
S. D. Anker, J. Butler, G. Filippatos, et al., “Empagliflozin in heart failure with a preserved ejection fraction,” New England Journal of Medicine, vol. 385, no. 16, pp. 1451-1461, 2021. https://doi.org/10.1056/NEJMoa2107038
S. D. Solomon, J. J. V. McMurray, B. Claggett, et al., “Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction,” New England Journal of Medicine, vol. 387, pp. 1089-1098, 2022. https://doi.org/10.1056/NEJMoa2206286
F. J. Forsyth, “PRESERVE HFpEF: Designing a blended lifestyle intervention to improve physical function, dietary intake, and quality of life in multi-morbid older people who have heart failure with preserved ejection fraction (HFpEF)” [doctoral dissertation], University of Cambridge (UK), 2024. https://doi.org/10.17863/CAM.115842
F. Epelde, “Optimizing cardiac rehabilitation in heart failure: comprehensive insights, barriers, and future strategies,” Medicina, vol. 60, no. 10, p. 1583, 2024. https://doi.org/10.3390/medicina601013
A. Aliyev, F. Ermatov, and O. Jo‘raboyev, “Advanced strategies in the management of chronic heart failure: a multidisciplinary and evidence-based approach,” Modern Science Research, vol. 4, no. 6, pp. 283-286, 2025.
A. Huitema, K. Haricness, G. Heckman, and R. S. McKelvie, “The spoke-hub-and-node model of integrated heart failure care,” Canadian Journal of Cardiology, vol. 34, no. 7, pp. 863-870, 2018. https://doi.org/10.1016/j.cjca.2018.03.002
L. Campbell-Williams, “Optimizing care for heart failure patients with reduced ejection fraction: a quality improvement project on guideline-directed medical therapy adherence,” Journal of Clinical Medicine, vol. 14, no. 4, p. 1050, 2025.
J. K. Dugal, A. S. Malhi, N. Ramazani, et al., “Non-pharmacological therapy in heart failure and management of heart failure in special populations—a review,” Journal of Clinical Medicine, vol. 13, no. 22, p. 6993, 2024. https://doi.org/10.3390/jcm13226993
S. Shah, B. Borlaug, D. Kitzman, et al., “Research priorities for heart failure with preserved ejection fraction: National Heart, Lung, and Blood Institute Working Group Summary,” Circulation, vol. 141, pp. 1001-1026, 2020. https://doi.org/10.1161/CIRCULATIONAHA.119.041886
S. J. Greene, J. Butler, N. M. Albert, et al., “Medical therapy for heart failure with reduced ejection fraction: the CHAMP-HF Registry,” Journal of the American College of Cardiology, vol. 72, pp. 351-369, 2018.
N. Shakour, S. Karami, M. Iranshahi, A. E. Butler, and A. Sahebkar, “Antifibrotic effects of sodium-glucose cotransporter-2 inhibitors: a comprehensive review,” Diabetes & Metabolic Syndrome: Clinical Research & Reviews, vol. 18, no. 1, p. 102934, 2024. https://doi.org/10.1016/j.dsx.2023.102934
J. Dyck, S. Sossalla, N. Hamdani, et al., “Cardiac mechanisms of the beneficial effects of SGLT2 inhibitors in heart failure: evidence for potential off-target effects,” Journal of Molecular and Cellular Cardiology, vol. 167, pp. 17-31, 2022. https://doi.org/10.1016/j.yjmcc.2022.03.005
M. M. Kittleson, G. S. Panjrath, K. Amancherla, et al., “2023 ACC expert consensus decision pathway on management of heart failure with preserved ejection fraction,” Journal of the American College of Cardiology, vol. 81, no. 18, pp. 1835-1878, 2023.
M. McDonald, S. Virani, M. Chan, et al., “CCS/CHFS Heart Failure Guidelines update: defining a new pharmacologic standard of care for heart failure,” Canadian Journal of Cardiology, vol. 37, pp. 531-546, 2021.
F. Zannad, J. P. Ferreira, S. J. Pocock, et al., “SGLT2 inhibitors in patients with heart failure: a meta-analysis of the EMPEROR-Reduced and DAPA-HF trials,” The Lancet, vol. 396, pp. 819-829, 2020.
H. G. C. Van Spall, T. Rahman, O. Mytton, et al., “Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta-analysis,” European Journal of Heart Failure, vol. 19, pp. 1427-1443, 2017.
M. Packer, S. Anker, J. Butler, et al., “Cardiovascular and renal outcomes with empagliflozin in heart failure,” New England Journal of Medicine, vol. 383, pp. 1413-1424, 2020. https://doi.org/10.1056/NEJMoa2022190
S. D. Solomon, R. A. de Boer, D. DeMets, et al., “Dapagliflozin in heart failure with preserved and mildly reduced ejection fraction: rationale and design of the DELIVER trial,” European Journal of Heart Failure, vol. 23, pp. 1217-1225, 2021. https://doi.org/10.1002/ejhf.2249
Y. Kubota and W. Shimizu, “Clinical benefits of sodium-glucose cotransporter 2 inhibitors and the mechanisms underlying their cardiovascular effects,” JACC: Asia, vol. 2, no. 3, pp. 287-293, 2022. https://doi.org/10.1016/j.jacasi.2022.03.009
P. Grubic Rotkvic, I. Celap, V. Bralic Lang, et al., “Impact of SGLT2 inhibitors on the mechanisms of myocardial dysfunction in type 2 diabetes: a prospective observational study,” Journal of Diabetes and its Complications, vol. 37, no. 8, p. 108541, 2023. https://doi.org/10.1016/j.jdiacomp.2023.108541
B. S. Alaujan, et al., “Integrating preventive cardiology in primary care: the role of nurses, pharmacists, health records, and emergency services,” International Journal of Health Sciences, vol. 5, suppl. 1, pp. 1049-1066, 2021.
N. Moghaddam, N. M. Hawkins, R. McKelvie, et al., “Patient eligibility for novel guideline-directed medical therapies after acute heart failure hospitalization,” JACC: Heart Failure, vol. 11, pp. 596-606, 2023.
M. Jarjour, C. Henri, S. de Denus, et al., “Care gaps in adherence to heart failure guidelines: clinical inertia or physiological limitations?” JACC: Heart Failure, vol. 8, pp. 725-738, 2020.
M. E. Nassif, S. L. Windsor, F. Tang, et al., “Dapagliflozin effects on biomarkers, symptoms, and functional status in heart failure with preserved ejection fraction: the PRESERVED-HF trial,” Circulation, vol. 144, no. 16, pp. 1284-1294, 2021. https://doi.org/10.1161/CIRCULATIONAHA.121.056824
E. I. Minsagirova, I. M. Sharafutdinov, M. L. Hossain, et al., “Comprehensive approach to the treatment of heart failure: integrating cardiology into medical care,” Revista Latinoamericana de Hipertensión, vol. 20, no. 2, 2025.
W. Raat, M. Smeets, S. Janssens, and B. Vaes, “Impact of primary care involvement and setting on multidisciplinary heart failure management: a systematic review and meta-analysis,” ESC Heart Failure, vol. 8, pp. 802-818, 2021. https://doi.org/10.1002/ehf2.13230
A. R. Barry, L. Kosar, S. L. Koshman, and R. D. Turgeon, “Medication management for heart failure: clinical pearls for optimizing therapy,” Canadian Family Physician, vol. 67, pp. 915-922, 2021.
A. Lopez-Usina, C. Mantilla-Cisneros, and J. Llerena-Velastegui, “Comprehensive benefits of sodium-glucose cotransporter 2 inhibitors in heart failure with reduced ejection fraction: a literature review,” Journal of Clinical Medicine Research, vol. 16, no. 10, p. 449, 2024. https://doi.org/10.14740/jocmr6033
J. Tromp, M. A. Khan, I. T. Klip, et al., “Biomarker profiles in heart failure patients with preserved and reduced ejection fraction,” Journal of the American Heart Association, vol. 6, no. 4, e003989, 2017. https://doi.org/10.1161/JAHA.116.003989
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Ayesha Shoukat, Mehvish Ambreen

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.


